The Positive Impact of EDI on CMS Compliance
Centers for Medicare and Medicaid Services (CMS) reporting requirements are designed to help ensure that healthcare providers and their contracted payers meet required standards and comply with Federal regulations. Manufacturers, medical equipment suppliers and other medical supply vendors may also be subject to reporting data to CMS.
The data these stakeholders report monitors the quality and efficiency of health-related services and products provided to Medicare and Medicaid recipients. The reports also provide checks and balances that these services are being delivered and are federally compliant.
Over the years, the number of Medicare and Medicaid beneficiaries has significantly increased as have the reporting requirements from CMS for reimbursements. The additional reporting requirements have brought new challenges to providers, payers, medical manufacturers and suppliers to be compliant.
These reporting requirements have impacted CMS participants in numerous ways.
- Increased Workloads – Providers, payers and others have had to devote more time and resources to gathering and organizing the required data for generating and submitting reports to CMS. These efforts add to their existing workloads and increase the time demands on their staff.
- Increased Costs – Time and allocating resources equates to increased costs. In addition, CMS participants may have to invest in licensing additional EDI-specific software and training for their staff.
- Increased Penalty Risk – Providing inaccurate data and incomplete reports subjects CMS participants to the risk of receiving penalties and other sanctions. These penalties can have significant financial consequences and impact an organization’s reputation.
It’s possible to meet CMS reporting requirements without EDI technology by transmitting data electronically, using specific formatting and meeting content requirements as dictated by CMS. To assist with this, CMS provides the specifications for electronic data submission. CMS specifications include the necessary use of specific data elements and codes. These specs must be rigorously followed for the data to be accepted and to avoid penalties.
For those not using EDI (Electronic Data Interchange) and who are electronically submitting data, you’ll need to ensure that it meets all CMS requirements and has the proper formatting. Submission may require some expertise and you may need to work with an experienced vendor or a third-party service provider who can help ensure you comply with all the CMS requirements.
While you do not need to use EDI technology, it is the preferred format for transmitting data to CMS because it offers the mechanisms required to exchange data securely and efficiently. Modern EDI solutions also provide the ability to validate data for accuracy before submission to help avoid compliance errors and any related CMS penalties.
EDI is a well-established standard for exchanging business data in a structured format. It uses a specific syntax and structure for the data, facilitating the exchange of data electronically rather than via paper documents. The syntax and structure are based on standards established by the American National Standards Institute (ANSI). The standard and the structure that EDI offers facilitate automating the process of exchanging data with payers and providers. By using EDI standards, payers, providers and others can save time and lower costs while also reducing errors.
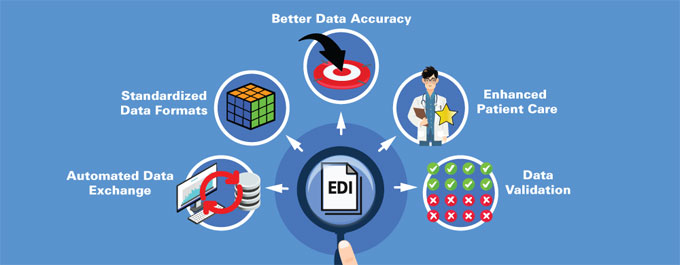
Overall, EDI technology has positively impacted how providers, payers and other CMS participants meet new CMS reporting requirements and can stay compliant with Federal laws for Medicare and Medicaid. Some of the specific areas where EDI has had a positive impact are:
- Automated Data Exchange – EDI solutions eliminate manual processing and enable the automation of data exchanged between healthcare providers, payers and others with CMS. EDI solutions help reduce the need for manual data entry, which minimizes errors. By reducing errors and improving data accuracy, EDI can facilitate compliance. Automation through an EDI solution also makes the process more efficient by allowing faster data transmission and fewer errors. Automation also allows the representative parties to use fewer human resources and lower costs.
- Standardized Data Formats – EDI solutions utilize standardized data formats and communications protocols for exchanging data. Using standardized EDI formats ensures that data is structured and organized consistently. Structure and the organization of data make it easier to understand and process the data. Standardization is particularly relevant when dealing with large amounts of data, which helps reduce errors and improve efficiency. Utilizing standardized data formats helps organizations meet the regulatory requirements for data quality and accuracy.
Using a standard format for data ensures that organizations provide complete and consistent data. Most importantly, it accurately reflects the information it intends to convey. Standardized data formats help ensure that the data being transmitted is in the correct format, meets the required CMS standards and is also compliant.
- Better Data Accuracy – Because EDI technology allows data to be transmitted and processed automatically, it eliminates the need for manual data entry. Better data accuracy is achieved by reducing the risk of errors caused by manual entry. Since X12 EDI transactions also include built-in checks to validate the transmitted data, it makes the data more accurate. The standardized formats that X12 EDI provides further help ensure data accuracy as data is consistently transmitted across different systems and organizations.
- Enhanced Patient Care – As the industry has moved away from Fee for Service (FFS) to quality measures, CMS has added precise reporting requirements related to the quality of patient care. EDI technology helps them achieve CMS quality measures. By providing more comprehensive and up-to-date patient records, EDI technology can help providers make better decisions and provide a higher level of patient care.
- Data Validation – EDI validation is the process of checking that EDI transactions (claims and other healthcare-related data exchanges) are correctly formatted and compliant with industry standards. EDI validation is a critical step in the process of meeting CMS Medicare and Medicaid reporting requirements because it helps ensure that the data submitted is accurate and complete. EDI validation also ensures that data can be appropriately processed and understood by all parties, CMS and trading partner systems. CMS may reject EDI transactions if they are not correctly validated, resulting in payment delays or other issues.
It is crucial for healthcare providers, payers and others to meet CMS Medicare and Medicaid reporting requirements to ensure that their EDI transactions are appropriately validated and that any errors or issues get addressed quickly. This process involves implementing and utilizing EDI validation tools and processes specifically designed for this purpose.
By providing a standardized and automated way to exchange data, it improves the accuracy of the data being transmitted. The data is further validated to make sure that it meets the required standards. This is how EDI technology helps organizations meet reporting requirements for Medicare and Medicaid, enabling CMS compliance.
PilotFish EDI Integration Solutions
Meeting Medicare and Medicaid requirements, as well as CMS compliance, is a complex process that can be made easier with modern EDI Solutions. PilotFish, Inc. does this as a provider of Electronic Data Interchange (EDI) solutions and services, specifically focused on the healthcare industry.
PilotFish’s comprehensive X12 EDI solution includes the eiPlatform, an enterprise integration solution and transactional integration system, the eiConsole for X12 EDI, the developer’s workstation featuring a graphical IDE (Integrated Development Environment) and the eiDashboard, a web-based application for transaction monitoring and operational Interface reporting & management.
The eiConsole for X12 EDI was specifically designed to address the complexities of working with Healthcare, HIPAA and Supply Chain EDI data. The eiConsole offers features and modules for parsing, validating, mapping and producing X12 EDI files. It provides a graphical user interface utilizing an Assembly Line process for building interfaces to and from trading partner systems.
Within the eiConsole, users can perform complex data mapping and transformations and end-to-end testing without any coding or scripting. The eiConsole has been specifically designed to make configuring, maintaining and managing interfaces easy to learn and easy to use. The Assembly Line process offers users an intuitive framework for working with interfaces and removes the dependencies on who created an interface to make it easier for teams to collaborate.
The many automated processes within the eiConsole, through configuration panels, drop-down menus and graphical drag & drop data mapping processes, significantly increases the speed with which interfaces can be configured and maintained. The efficiency, made possible with the eiConsole, allows an organization to have smaller teams with lower overhead costs.
PilotFish, as a licensed distribution partner of X12, has been authorized to redistribute artifacts of the X12 standard. The eiConsole for X12 EDI also includes a rules-driven EDI SNIP Validation Processor for validating SNIP Types 1-7 (SNIP Levels) and users can optionally license code maintenance.
In summary, PilotFish offers a comprehensive EDI solution for the healthcare industry that provides everything needed to meet Medicare and Medicaid requirements and CMS compliance. Contact us to set up a demo or read our X12 EDI Case Studies and learn how clients leverage PilotFish as an EDI Solution.
If you’re curious about the software features, free trial, or even a demo – we’re ready to answer any and all questions. Please call us at 860 632 9900 or click the button.

